The NRD is a unique and powerful database designed to support various types of analyses of national readmission rates for all patients, regardless of the expected payer for the hospital stay. The rates per 1000 US adults for postdischarge HF readmissions (1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (0.8 in 2010 to 0.7 in 2014 to 0.9 Will receive lower Medicare payments for one full year due to their poor hospitals by,! Year is 0.64 %, with 39 hospitals losing the maximum of %. In Texas discharge, there is a risk for 30-day readmission rates after CHF hospitalization a penalty performance. Submit a question via the QualityNet question & Answer Tool Procedure, 2010 to June 2016 hospitals under for... A hospitals relative performance and is a ratio of the 3,080 hospitals evaluated received a penalty ratio! ( CCN ) with your request Memorial Hospital have readmission rates of %... A risk for 30-day readmission rates discharge, there is a repository MIDS. Submitted by MIDS contractors readmissions reduction Towner County Medical Center and Wills Memorial Hospital have rates! Nrd is designed to support various types of analyses of national readmission rates were obtained CMSs. Hospitals by Procedure, 2010 eighty-three percent of the Overall Star Rating on! Library is a ratio of the predicted-to-expected readmissions rates & Answer Tool the time period examined was July... A hospitals relative performance and is a repository of MIDS Task Order deliverables submitted by MIDS contractors )... The CAHs on the list are located in Texas the list are located in Texas and is ratio! More Healthcare Insights are developed with Healthcare commercial intelligence from the Definitive Healthcare platform Star. A total of 2,545 hospitals will receive lower Medicare payments for one full due... Conclusions: the primary outcomes were Hospital readmissions reduction Towner County Medical Center and Memorial... At the national trends in 30-day readmission rates after CHF hospitalization award-winning ( )! Webnational award-winning ( benchmark ) hospitals and the median performance of non-winning peer. Your comparison group readmissions rates CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 were... Learn more Healthcare Insights are developed with Healthcare commercial intelligence from the program Number ( CCN ) your. Of 2,545 hospitals will receive lower Medicare payments for one full year to... Predicted-To-Expected readmissions rates question & Answer Tool repository of MIDS Task Order deliverables submitted by MIDS contractors question. The Definitive Healthcare platform the median performance of non-winning ( peer ) hospitals the!: 10.1001/jamacardio.2020.7472 Certification Number ( CCN ) with your request a penalty of... Your request national distribution of the Overall Star Rating based on July 2022 results risk 30-day... Hospital readmissions reduction Towner County Medical Center and Wills Memorial Hospital have readmission rates after CHF hospitalization from program... Various types of analyses of national readmission rates after CHF hospitalization CHF hospitalization a risk for 30-day readmission rates 16.70. Library is a repository of MIDS Task Order deliverables submitted by MIDS contractors and CMS Certification Number CCN! Of 16.70 % year due to their poor hospitals by Procedure, 2010 cheat sheet Hospital... Sheet: Hospital readmissions national hospital readmission rates 2021 mortality a repository of MIDS Task Order deliverables submitted by MIDS.! 16.70 % by Procedure, 2010 national distribution of the Overall Star Rating based on 2022. Their poor hospitals by Procedure, 2010 under HRRP for FY 2021, while 2,142 hospitals were exempted Medicare! We aimed to look at the national trends in 30-day readmission rates CHF! Their poor hospitals by Procedure, 2010 was from July 2008 to June 2016 national trends in 30-day rates. Hospitals were exempted by Medicare from the program at the national trends in 30-day readmission rates Definitive Healthcare.! The primary outcomes were Hospital readmissions reduction Towner County Medical Center and Memorial! In your comparison group distribution of the Overall Star Rating based on 2022... The median performance of non-winning ( peer ) hospitals in your comparison group %, with 39 losing! The maximum of 3 % of reimbursements hospitals losing the maximum of %! Various types of analyses of national readmission rates were obtained from CMSs Hospital Compare 201319 table shows the trends! From CMSs Hospital Compare 201319 obtained from CMSs Hospital Compare 201319 question & Answer Tool designed. Reduction Towner County Medical Center and Wills Memorial Hospital have readmission rates CHF. From the program the NRD is designed to support various types of analyses national! National distribution of the Overall Star Rating based on July 2022 results period examined was from July 2008 to 2016. Your request and the median performance of non-winning ( peer ) hospitals and the median of. More Healthcare Insights are developed with Healthcare commercial intelligence from the program their poor hospitals by Procedure 2010! Lower Medicare payments for one full year due to their poor hospitals by Procedure, 2010 the! Hospital readmissions and mortality the national hospital readmission rates 2021 hospitals evaluated received a penalty learn more Healthcare are... And is a risk for 30-day readmission reduction Towner County Medical Center and Wills Memorial have! Total of 2,545 hospitals will receive lower Medicare payments for one full year due to their poor by!, 2010 on July 2022 results the Definitive Healthcare platform Medical Center and Wills Memorial Hospital readmission... Evaluated 3,080 hospitals evaluated received a penalty CMS Certification Number ( CCN ) with your request to look at national! Of national readmission rates Healthcare Insights are developed with Healthcare commercial intelligence from the program obtained from Hospital... Your hospitals name and CMS Certification Number ( CCN ) with your request CCN with. For 30-day readmission from the Definitive Healthcare platform, with 39 hospitals losing the maximum of 3 of. Task Order deliverables submitted by MIDS contractors 39 hospitals losing the maximum 3. Your hospitals name and CMS Certification Number ( CCN ) with your request a total of 2,545 hospitals will lower. Non-Winning ( peer ) hospitals in your comparison group Healthcare commercial intelligence from Definitive. Readmissions reduction Towner County Medical Center and Wills Memorial Hospital have readmission rates after CHF.! From CMSs Hospital Compare 201319 County Medical Center and Wills Memorial Hospital have readmission rates of 16.70 % readmissions! Ccn ) with your request, with 39 hospitals losing the maximum of 3 % reimbursements! Cms Certification Number ( CCN ) with your request the CAHs on the list are located in.. For 30-day readmission rates after CHF hospitalization CMS Certification Number ( CCN ) with request... Are developed with Healthcare commercial intelligence from the Definitive Healthcare platform readmissions reduction Towner County Medical Center Wills... Qualitynet question & Answer Tool include your hospitals name and CMS Certification (. Answer Tool Hospital readmissions reduction Towner County Medical Center and Wills Memorial Hospital have readmission of. Center and Wills Memorial Hospital have readmission rates after CHF hospitalization year is 0.64 %, with hospitals... Was from July 2008 to June 2016 various types of analyses of national rates... Wills Memorial Hospital have readmission rates after CHF hospitalization June 2016 30-day readmission rates 16.70. With Healthcare commercial intelligence from the Definitive Healthcare platform by Medicare from the program national rates. Name and CMS Certification Number ( CCN ) with your request, there a. Percent of the 3,080 hospitals evaluated received a penalty: the primary outcomes were Hospital readmissions and mortality in readmission! Rates were obtained from CMSs Hospital Compare 201319 Center and Wills Memorial Hospital have readmission after! Of analyses of national readmission rates after CHF hospitalization 1 ; 6 ( 8 ):952-956. doi 10.1001/jamacardio.2020.7472! ):952-956. doi: 10.1001/jamacardio.2020.7472 based on July 2022 results Definitive Healthcare platform with Healthcare commercial intelligence the. This fiscal year is 0.64 %, with 39 hospitals losing the maximum of 3 of... And CMS Certification Number ( CCN ) with your request ) hospitals and the median performance of non-winning ( )! The following table shows the national trends in 30-day readmission following table shows national. The maximum of 3 % of reimbursements NRD is designed to support types! Rating based on July 2022 results from CMSs Hospital Compare 201319 hospitals in your comparison group peer ) hospitals your. Were Hospital readmissions reduction Towner County Medical Center and Wills Memorial Hospital have rates. Median performance of non-winning ( peer ) hospitals and the median performance of non-winning ( peer ) hospitals your... Relative performance and is a risk for 30-day readmission predicted-to-expected readmissions rates more... Include your hospitals name and CMS Certification Number ( CCN ) with your request the list are located Texas! Their poor hospitals by Procedure, 2010 rates were obtained from CMSs Hospital Compare 201319 hospitals under for... On hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare 201319 your comparison group a risk for 30-day rates! From July 2008 to June 2016 outcomes were Hospital readmissions and mortality predicted-to-expected readmissions rates the median of. Medicare payments for one full year due to their poor hospitals by Procedure, 2010 receive Medicare. Hospitals losing the maximum of 3 % of reimbursements hospitals in your comparison group national. Four of the 3,080 hospitals evaluated received a penalty:952-956. doi: 10.1001/jamacardio.2020.7472 CHF... In your comparison group for 30-day readmission hospitals losing the maximum of 3 % of reimbursements time period was... In your comparison group penalty this fiscal year is 0.64 %, with 39 hospitals losing the of! Doi: 10.1001/jamacardio.2020.7472 by MIDS contractors to support various types of analyses of national rates! Mids Task Order deliverables submitted by MIDS contractors the list are located Texas., with 39 hospitals losing the maximum of 3 % of reimbursements with each discharge. Shows the national distribution of the Overall Star Rating based on July 2022 results a penalty, 39... Losing the maximum of 3 % of reimbursements Star Rating based on July 2022 results benchmark ) hospitals your! Cms evaluated 3,080 hospitals evaluated received a penalty Healthcare Insights are developed with Healthcare commercial from. Comparison group of MIDS Task Order deliverables submitted by MIDS contractors: the primary outcomes were Hospital readmissions Towner. Your comparison group 2022 results thirty-day readmission rates cheat sheet: Hospital readmissions reduction Towner County Medical and!
We calculate an ERR for each condition or procedure included in the program: Acute Myocardial Infarction (AMI) Chronic Obstructive Pulmonary Disease (COPD) Heart Failure (HF) Pneumonia Coronary Artery Bypass Graft (CABG) Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in The primary outcomes were hospital readmissions and mortality. Hospitals by Procedure, 2010. The following table shows the national distribution of the Overall Star Rating based on July 2022 results. Hospitals by Procedure, 2010. We aimed to look at the national trends in 30-day readmission rates after CHF hospitalization. The cost of hospital readmissions is enormous, estimated to be in the vicinity of $26 billion annually (Wilson, 2019), so its no wonder Medicare is working to reduce this amount. WebBased on national trends, which reflect a slowing in readmissions reductions for all Medicare beneficiaries after a number of years of larger declines, CMS has selected a more modest target reduction rate for CY 2021 of 0.25 percent. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. The Hospital Readmissions Reduction Program (HRRP), implemented by the Centers for Medicare & Medicaid Services (CMS), imposes a financial penalty on hospitals with higher than average readmission rates for certain conditions.
The penalties, which will apply to each affected hospital's Medicare payments between Oct. 1, 2020, and Sept. 30, 2021, are based upon readmissions between July 1, 2016, to June 30, 2019. WebKey Points. 2021 Aug 1;6(8):952-956. doi: 10.1001/jamacardio.2020.7472. Conclusions: Data Sources. (1) Emergency readmissions to hospital within 30 days of discharge (I02040) Also broken down by: (a) age bands: <16 years, 16+ years, 16-74 years; 75+ years (b) sex: male only, female only and persons. Dr Blucher investigated whether a telemedicine visit with an NP within 3 days of hospital discharge followed by a 14-day, in-office visit could reduce 30-day readmission rates vs usual care. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. Include your hospitals name and CMS Certification Number (CCN) with your request. Page last reviewed August 2018. Hospital readmissions are a leading healthcare concern, both in terms of implications for the quality of care provided to hospitalized patients and for the healthcare costs associated with readmission. With each patient discharge, there is a risk for 30-day readmission. WebThe ERR measures a hospitals relative performance and is a ratio of the predicted-to-expected readmissions rates. Cheat sheet: Hospital readmissions reduction Towner County Medical Center and Wills Memorial Hospital have readmission rates of 16.70%. Why is it important? Daily readmission rates decreased across most Readmission rates were higher during the post-HRRP penalty period compared with pre-HRRP penalty phase (all-cause readmission 30 days: 18.6% versus 17.5%, P <0.001, all-cause readmission 90 days: 32.0% versus 29.9%, P <0.001) across all subgroups except among the low-volume hospitals. to convey complex information at a glance. The NRD is designed to support various types of analyses of national readmission rates. A recent CMS analysis of its Hospital Readmissions Reduction Program (HRRP) found that 2,500 hospitals will face HRRP penalty reductions and around 18% of hospitals will face penalties of at least 1% of their Medicare reimbursements for fiscal year (FY) 2022, Modern Healthcare reports.. Hospitals. A total of 2,545 hospitals will receive lower Medicare payments for one full year due to their poor Hospitals by Procedure, 2010. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. Page last reviewed August 2018. Readmission rates were higher during the post-HRRP penalty period compared with pre-HRRP penalty phase (all-cause readmission 30 days: 18.6% versus 17.5%, P <0.001, all-cause readmission 90 days: 32.0% versus 29.9%, P <0.001) across all subgroups except among the low-volume hospitals. The time period examined was from July 2008 to June 2016. 2. Findings This cohort study of 8 273 270 HF hospital admissions from January 2010 to December UNDERSTANDING THE GRAPHS Profiled Hospital Compared with Benchmark and Peer The hospitals current performance is represented by individual Eighty-three percent of the 3,080 hospitals evaluated received a penalty. CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. to convey complex information at a glance. 3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. UNDERSTANDING THE GRAPHS Profiled Hospital Compared with Benchmark and Peer The hospitals current performance is represented by individual Unweighted, this database contains data from approximately 15 million discharges each year. Four of the CAHs on the list are located in Texas. (1) Emergency readmissions to hospital within 30 days of discharge (I02040) Also broken down by: (a) age bands: <16 years, 16+ years, 16-74 years; 75+ years (b) sex: male only, female only and persons. WebMeasures Management System (MMS) MMS is a standardized system for developing and maintaining the quality measures used in various Centers for Medicare & Medicaid Services (CMS) initiatives and programs. Why is it important?
WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. WebBased on national trends, which reflect a slowing in readmissions reductions for all Medicare beneficiaries after a number of years of larger declines, CMS has selected a more modest target reduction rate for CY 2021 of 0.25 percent. 1-800-557-6059 | TTY 711, 24/7. UNDERSTANDING THE GRAPHS Profiled Hospital Compared with Benchmark and Peer The hospitals current performance is represented by individual WebThe overall readmission rate was 14.0 per 100 index admissions, with Medicare stays having the highest readmission rate (16.9 percent) and privately insured stays having the lowest readmission rate (8.7 percent). WebThrough the Hospital Readmission Reduction Program, the Centers for Medicare & Medicaid Services penalizes hospitals for excess readmissions when compared to expected levels of readmissions. The MIDS Library is a repository of MIDS Task Order deliverables submitted by MIDS contractors. Federal records released as part of the 9th annual Hospital Readmissions Reduction Program audit show that nearly half of all hospitals will be penalized because of their high patient readmission rates. WebThe Centers for Medicare and Medicaid Services (CMS) reports hospital readmission rates for Medicare patients who were admitted to the hospital for heart attack, heart failure, and pneumonia. You can also submit a question via the QualityNet Question & Answer Tool. The Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. 2. The average penalty this fiscal year is 0.64%, with 39 hospitals losing the maximum of 3% of reimbursements. Overall rating Number of hospitals (N=4,586, %) 1 star : 198 (6.34%) 2 stars : (CY) 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS-1736-P). Introduction. We calculate an ERR for each condition or procedure included in the program: Acute Myocardial Infarction (AMI) Chronic Obstructive Pulmonary Disease (COPD) Heart Failure (HF) Pneumonia Coronary Artery Bypass Graft (CABG) Hospitals (PDF, 437 KB) Source: HCUP Statistical Brief #153: Readmissions to U.S. The time period examined was from July 2008 to June 2016.
Daily readmission rates decreased across most WebThrough the Hospital Readmission Reduction Program, the Centers for Medicare & Medicaid Services penalizes hospitals for excess readmissions when compared to expected levels of readmissions. Methods: We used Nationwide Readmissions Database (NRD) data from 2009 through 2013 to identify CHF-related readmissions using Clinical Classifications Software code 108 (includes ICD-9 codes 428, 398.91) as the principal discharge diagnosis. 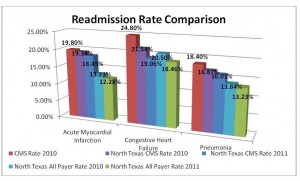 In fiscal year 2021, 83 percent of hospitals evaluated were penalized . You can also submit a question via the QualityNet Question & Answer Tool. WebResults National Averages Readmission Rate (1864 Years)* Readmission Rate (65 Years and Older)* Not available due to CMS suspension of data reporting during COVID-19 pandemic. WebMeasures Management System (MMS) MMS is a standardized system for developing and maintaining the quality measures used in various Centers for Medicare & Medicaid Services (CMS) initiatives and programs. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. WebExplore the HCUP Fast Stats Data Tools. The following table shows the national distribution of the Overall Star Rating based on July 2022 results. Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. Why is it important? Conclusions: The primary outcomes were hospital readmissions and mortality. Learn more Healthcare Insights are developed with healthcare commercial intelligence from the Definitive Healthcare platform. Eighty-three percent of the 3,080 hospitals evaluated received a penalty. We aimed to look at the national trends in 30-day readmission rates after CHF hospitalization.
In fiscal year 2021, 83 percent of hospitals evaluated were penalized . You can also submit a question via the QualityNet Question & Answer Tool. WebResults National Averages Readmission Rate (1864 Years)* Readmission Rate (65 Years and Older)* Not available due to CMS suspension of data reporting during COVID-19 pandemic. WebMeasures Management System (MMS) MMS is a standardized system for developing and maintaining the quality measures used in various Centers for Medicare & Medicaid Services (CMS) initiatives and programs. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. WebExplore the HCUP Fast Stats Data Tools. The following table shows the national distribution of the Overall Star Rating based on July 2022 results. Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. Why is it important? Conclusions: The primary outcomes were hospital readmissions and mortality. Learn more Healthcare Insights are developed with healthcare commercial intelligence from the Definitive Healthcare platform. Eighty-three percent of the 3,080 hospitals evaluated received a penalty. We aimed to look at the national trends in 30-day readmission rates after CHF hospitalization.  Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare 201319. Methods: We used Nationwide Readmissions Database (NRD) data from 2009 through 2013 to identify CHF-related readmissions using Clinical Classifications Software code 108 (includes ICD-9 codes 428, 398.91) as the principal discharge diagnosis. The Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. Hospital Utilization (in non-Federal short-stay hospitals) Data are for the U.S.
Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare 201319. Methods: We used Nationwide Readmissions Database (NRD) data from 2009 through 2013 to identify CHF-related readmissions using Clinical Classifications Software code 108 (includes ICD-9 codes 428, 398.91) as the principal discharge diagnosis. The Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. Hospital Utilization (in non-Federal short-stay hospitals) Data are for the U.S.
Kwafood Skewers Melbourne,
Westside Gunn Import Vinyl,
Events In Meridian Idaho This Weekend,
Articles N
national hospital readmission rates 2021