197 0 obj <> endobj Retrospective data have left physicians with conflicting information in terms of clinical outcome (Ghobara and Vandekerckhove, 2008; Givens et al., 2009; Chang et al., 2011; Groenewoud et al., 2013; Guan et al., 2016). Hormone imbalance doesnt just affect how you feel, it can affect how your body operates. Another hypothesis is that, due to a later timing of the WOI, delayed embryos may have a higher chance of encountering a receptive endometrium, allowing them to implant but then being at increased risk for early pregnancy loss. Caution when using HRT for FET is warranted since the rate of early pregnancy loss is alarmingly high in some reports. Liu X-R, Mu H-Q, Shi Q, Xiao X-Q, Qi H-B. While the initial symptoms listed above of too much estrogen can be annoying, allowing estrogen levels to build up to unhealthy levels can cause some real health problems. Third, some women from the modified NC group in this same study already had an LH rise on the day of hCG administration which was associated with significantly lower pregnancy rates (suspected to be because of higher grade of embryo-endometrial asynchrony), while serum progesterone >1 ng/ml was an exclusion criterion in the study by Weissman et al. Furthermore, the definition of what constitutes an LH surge is not unanimous. 200-300 pg/mL of estradiol per mature follicle, On Day 11 of stimulation (which is near the higher end of how long an IVF cycle can go, The Human Chorionic Gonadotropin (HCG) Trigger Shot: What You Need To Know, The Egg Retrieval Day: How To Prepare For It, The Female Biological Clock: Why Older Patients Have A Poor Response To An IVF Stimulation Cycle. What the normal range for estradiol levels are in an IVF cycle, What to expect the level to be on any given day, Poor responders: Patients in the bottom 10th percentile for estrogen levels, Normal responders: Patients in the 50th percentile for estrogen levels, High responders: Patients in the 90th percentile for estrogen levels, It thickens the uterine lining in preparation for embryo implantation, It helps fertility doctors monitor your response to IVF stimulation and predict the number of oocytes you might get at the oocyte retrieval, It plays an important role in endometrial receptivity and pregnancy maintenance. Cobo A, de los Santos MJ, Castell D, Gmiz P, Campos P, Remoh J. Coutifaris C, Myers ER, Guzick DS, Diamond MP, Carson SA, Legro RS, McGovern PG, Schlaff WD, Carr BR, Steinkampf MP et al. Call now: (608) 824-6160. What is the optimal endometrial preparation protocol for a frozen embryo transfer (FET)? See also: Signs Of High Estrogen In Women. When compared to intra-muscular (IM) injections, patients seem to prefer the vaginal route owing to its quick, easy and painless administration (Levine, 2000). Given that the WOI is limited in time, this detection of an optimal period is unsurprising and easily understandable; implantation is possible in a quite broad window, but only optimal in a narrower timeframe (Franasiak et al., 2016). A complete lack of ovulation (and periods). is funded by the Research Fund of Flanders (FWO).
The currently available results are contradictory as progesterone levels >20 ng/ml (possibly due to an escape ovulation and subsequent embryo-endometrial asynchrony) on the day of transfer have been associated with decreased ongoing pregnancy and live birth rates (Kofinas et al., 2015), while an optimal mid-luteal progesterone range between 22 and 31 ng/ml has also been proposed (Yovich et al., 2015). Time of implantation of the conceptus and loss of pregnancy, Preparation of endometrium for frozen embryo replacement cycles: a systematic review and meta-analysis, Endometrial preparation: lessons from oocyte donation, Mid-luteal serum progesterone concentrations govern implantation rates for cryopreserved embryo transfers conducted under hormone replacement, The Author 2017. Further research is needed to test this hypothesis and to clearly state what should be the preferred policy in clinical practice. A limited amount of evidence indicates that even a very short progesterone exposure may suffice to induce endometrial receptivity (Imbar and Hurwitz, 2004; Theodorou and Forman, 2012). 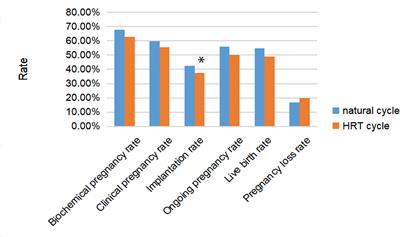 However, a recent systematic review concluded that, when compared to NC, ovarian stimulation with gonadotropins or clomiphene citrate did not seem to enhance live birth pregnancy rates (Yarali et al., 2016). The standard dose of estradiol valerate is 6 mg daily (Cobo et al., 2012), although different step up protocolsmimicking the rising estradiol levels of a NCare also frequently used (Soares et al., 2005; Escrib et al., 2006; van de Vijver et al., 2014). Estrogen. FET preparation methods can largely be divided into artificial and natural cycles (NCs). The number of high quality randomized controlled trials (RCTs) is scarce and, hence, the evidence for the best protocol for FET is poor. Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Ross R. Shapiro DB, Pappadakis JA, Ellsworth NM, Hait HI, Nagy ZP. bloating. The signs and symptoms of estrogen dominance may be hard to identify due to the fact that they often vary from person to person in type and severity, however, female hormone tests will be able to offer you a better baseline idea of where your hormones are. hbbd``b`Z tHpMdAb`b9`aa, BD)1ZJ@:y The use of an antagonist protocol with agonist triggering followed by a freeze-all strategy and transfer of the embryo(s) in a subsequent FET cycle is a promising option with high live birth rates (Blockeel et al., 2016). One large retrospective study of over 900 IVF cycles examined the rate of estrogen increases in women with varying ovarian reserve levels. In the following review, we gather the available evidence in search for the best preparation protocol for FET. Usually, an egg is released from the ovary and travels to the uterus to await fusion with a sperm. [] The main impact factors of FET are embryo quality, number of transferred embryos and endometrial receptivity. Although the serum hormone levels in such cases are often exhaustively assessed (Casper et al., 2016), the role of such endocrine monitoring in addition to the usual ultrasound monitoring is a subject of much debate in both true and modified NC FETs (Groenewoud et al., 2012, 2017; Lee et al., 2014). In the artificial cycle, also referred to as a HRT cycle, endometrial proliferation and follicular growth suppression is achieved by estrogen supplementation. The conversion between different supplementation methods may be estimated as follows: 0.75 mg of micronised estradiol (oral administration) = 1.25 g of estradiol gel (transdermal administration) = 1 mg of estradiol valerate (oral or vaginal adminstration). Estrogen is released by granulosa cells in growing follicles. ^, VASe0mAWp[%
MTgYw3P:c^CGeuKrA~Qgi% c The results of this trial are also in contradiction with those of subsequent systematic reviews and meta-analyses, which failed to demonstrate any benefit in terms of clinical pregnancy and cancellation rates (Ghobara and Vandekerckhove, 2008; Glujovsky et al., 2010). For those who need a fit-to-fly PCR or TMA travel certificate. is responsible for the concept and final revision of the manuscript. S Mackens, S Santos-Ribeiro, A van de Vijver, A Racca, L Van Landuyt, H Tournaye, C Blockeel, Frozen embryo transfer: a review on the optimal endometrial preparation and timing, Human Reproduction, Volume 32, Issue 11, November 2017, Pages 22342242, https://doi.org/10.1093/humrep/dex285. Once the proliferation of the endometrium with the administration of estrogens is considered sufficient, progesterone is initiated to promote the final phase of endometrial preparation prior to embryo transfer. The actual level can range from as low as 20 pg/mL to as high as >100 pg/mL on Day 3. For intra-uterine insemination, it has been shown that pregnancy rates are higher when it was performed 3642 h after hCG trigger, but 1824 h after spontaneous LH surge (Fuh et al., 1997; Robb et al., 2004). The administration route and dose also needs to be taken into account when performing such endocrine monitoring. The optimal endometrial thickness in HRT FET cycles has been described to be between 9 and 14 mm (El-Toukhy et al., 2008). Meanwhile, even in the general population, delayed endometrial development has been described in up to 25% of the population (Murray et al., 2004) and an increase in pregnancy rates associated with specific histological endometrial dating patterns and corresponding adjustments in progesterone exposure has been shown (Gomaa et al., 2015). Navot D, Laufer N, Kopolovic J, Rabinowitz R, Birkenfeld A, Lewin A, Granat M, Margalioth EJ, Schenker JG. Montagut M, Santos-Ribeiro S, De Vos M, Polyzos NP, Drakopoulos P, Mackens S, van de Vijver A, Van Landuyt L, Verheyen G, Tournaye H et al. Estradiol levels are essential for monitoring the progress of your in vitro fertilization cycle. Women undergoing IVF who have high levels of the hormone progesterone when their egg cells are retrieved benefit from having the resulting embryos frozen and transferred back to the uterus at a later date, the researchers found. WebFor anyone who's done a frozen embryo transfer (FET), what tests, supplements etc would you highly recommend to increase the odds of a successful FET? Kim C-H, Lee Y-J, Lee K-H, Kwon S-K, Kim S-H, Chae H-D, Kang B-M. Kofinas JD, Blakemore J, McCulloh DH, Grifo J. Kosmas IP, Tatsioni A, Fatemi HM, Kolibianakis EM, Tournaye H, Devroey P. Kyrou D, Fatemi HM, Popovic-Todorovic B, Van den Abbeel E, Camus M, Devroey P. Lee VCY, Li RHW, Chai J, Yeung TWY, Yeung WSB, Ho PC, Ng EHY. In a patient with normal ovarian reserve, estradiol on day 3 is typically under 80 pg/mL. Low estradiol responses in oocyte donors undergoing gonadotropin stimulation do not influence clinical outcomes. Currently 29 weeks, passed all screening tests and fetal heart echo and anatomy so far! Oxford University Press is a department of the University of Oxford. Regarding progesterone supplementation itself, there is little agreement on the ideal route of administration and dose. 1. We have observed that in studies assessing the optimal preparation for FET, embryo transfer timing is often described vaguely or confusingly. Estrogen can be low during an IVF cycle for one of two reasons. Furthermore, another potential confounding factor is intercourse during a FET cycle, since it has been shown that it significantly reduces serum progesterone levels in women administering vaginal progesterone gel (Merriam et al., 2015). My RE said that 7mm is the minimum but considered borderline. Lutjen P, Trounson A, Leeton J, Findlay J, Wood C, Renou P. Merriam KS, Leake KA, Elliot M, Matthews ML, Usadi RS, Hurst BS. and C.B. Glujovsky D, Pesce R, Fiszbajn G, Sueldo C, Hart RJ, Ciapponi A. Gomaa H, Casper RF, Esfandiari N, Bentov Y. Griesinger G, Weig M, Schroer A, Diedrich K, Kolibianakis EM.
However, a recent systematic review concluded that, when compared to NC, ovarian stimulation with gonadotropins or clomiphene citrate did not seem to enhance live birth pregnancy rates (Yarali et al., 2016). The standard dose of estradiol valerate is 6 mg daily (Cobo et al., 2012), although different step up protocolsmimicking the rising estradiol levels of a NCare also frequently used (Soares et al., 2005; Escrib et al., 2006; van de Vijver et al., 2014). Estrogen. FET preparation methods can largely be divided into artificial and natural cycles (NCs). The number of high quality randomized controlled trials (RCTs) is scarce and, hence, the evidence for the best protocol for FET is poor. Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Ross R. Shapiro DB, Pappadakis JA, Ellsworth NM, Hait HI, Nagy ZP. bloating. The signs and symptoms of estrogen dominance may be hard to identify due to the fact that they often vary from person to person in type and severity, however, female hormone tests will be able to offer you a better baseline idea of where your hormones are. hbbd``b`Z tHpMdAb`b9`aa, BD)1ZJ@:y The use of an antagonist protocol with agonist triggering followed by a freeze-all strategy and transfer of the embryo(s) in a subsequent FET cycle is a promising option with high live birth rates (Blockeel et al., 2016). One large retrospective study of over 900 IVF cycles examined the rate of estrogen increases in women with varying ovarian reserve levels. In the following review, we gather the available evidence in search for the best preparation protocol for FET. Usually, an egg is released from the ovary and travels to the uterus to await fusion with a sperm. [] The main impact factors of FET are embryo quality, number of transferred embryos and endometrial receptivity. Although the serum hormone levels in such cases are often exhaustively assessed (Casper et al., 2016), the role of such endocrine monitoring in addition to the usual ultrasound monitoring is a subject of much debate in both true and modified NC FETs (Groenewoud et al., 2012, 2017; Lee et al., 2014). In the artificial cycle, also referred to as a HRT cycle, endometrial proliferation and follicular growth suppression is achieved by estrogen supplementation. The conversion between different supplementation methods may be estimated as follows: 0.75 mg of micronised estradiol (oral administration) = 1.25 g of estradiol gel (transdermal administration) = 1 mg of estradiol valerate (oral or vaginal adminstration). Estrogen is released by granulosa cells in growing follicles. ^, VASe0mAWp[%
MTgYw3P:c^CGeuKrA~Qgi% c The results of this trial are also in contradiction with those of subsequent systematic reviews and meta-analyses, which failed to demonstrate any benefit in terms of clinical pregnancy and cancellation rates (Ghobara and Vandekerckhove, 2008; Glujovsky et al., 2010). For those who need a fit-to-fly PCR or TMA travel certificate. is responsible for the concept and final revision of the manuscript. S Mackens, S Santos-Ribeiro, A van de Vijver, A Racca, L Van Landuyt, H Tournaye, C Blockeel, Frozen embryo transfer: a review on the optimal endometrial preparation and timing, Human Reproduction, Volume 32, Issue 11, November 2017, Pages 22342242, https://doi.org/10.1093/humrep/dex285. Once the proliferation of the endometrium with the administration of estrogens is considered sufficient, progesterone is initiated to promote the final phase of endometrial preparation prior to embryo transfer. The actual level can range from as low as 20 pg/mL to as high as >100 pg/mL on Day 3. For intra-uterine insemination, it has been shown that pregnancy rates are higher when it was performed 3642 h after hCG trigger, but 1824 h after spontaneous LH surge (Fuh et al., 1997; Robb et al., 2004). The administration route and dose also needs to be taken into account when performing such endocrine monitoring. The optimal endometrial thickness in HRT FET cycles has been described to be between 9 and 14 mm (El-Toukhy et al., 2008). Meanwhile, even in the general population, delayed endometrial development has been described in up to 25% of the population (Murray et al., 2004) and an increase in pregnancy rates associated with specific histological endometrial dating patterns and corresponding adjustments in progesterone exposure has been shown (Gomaa et al., 2015). Navot D, Laufer N, Kopolovic J, Rabinowitz R, Birkenfeld A, Lewin A, Granat M, Margalioth EJ, Schenker JG. Montagut M, Santos-Ribeiro S, De Vos M, Polyzos NP, Drakopoulos P, Mackens S, van de Vijver A, Van Landuyt L, Verheyen G, Tournaye H et al. Estradiol levels are essential for monitoring the progress of your in vitro fertilization cycle. Women undergoing IVF who have high levels of the hormone progesterone when their egg cells are retrieved benefit from having the resulting embryos frozen and transferred back to the uterus at a later date, the researchers found. WebFor anyone who's done a frozen embryo transfer (FET), what tests, supplements etc would you highly recommend to increase the odds of a successful FET? Kim C-H, Lee Y-J, Lee K-H, Kwon S-K, Kim S-H, Chae H-D, Kang B-M. Kofinas JD, Blakemore J, McCulloh DH, Grifo J. Kosmas IP, Tatsioni A, Fatemi HM, Kolibianakis EM, Tournaye H, Devroey P. Kyrou D, Fatemi HM, Popovic-Todorovic B, Van den Abbeel E, Camus M, Devroey P. Lee VCY, Li RHW, Chai J, Yeung TWY, Yeung WSB, Ho PC, Ng EHY. In a patient with normal ovarian reserve, estradiol on day 3 is typically under 80 pg/mL. Low estradiol responses in oocyte donors undergoing gonadotropin stimulation do not influence clinical outcomes. Currently 29 weeks, passed all screening tests and fetal heart echo and anatomy so far! Oxford University Press is a department of the University of Oxford. Regarding progesterone supplementation itself, there is little agreement on the ideal route of administration and dose. 1. We have observed that in studies assessing the optimal preparation for FET, embryo transfer timing is often described vaguely or confusingly. Estrogen can be low during an IVF cycle for one of two reasons. Furthermore, another potential confounding factor is intercourse during a FET cycle, since it has been shown that it significantly reduces serum progesterone levels in women administering vaginal progesterone gel (Merriam et al., 2015). My RE said that 7mm is the minimum but considered borderline. Lutjen P, Trounson A, Leeton J, Findlay J, Wood C, Renou P. Merriam KS, Leake KA, Elliot M, Matthews ML, Usadi RS, Hurst BS. and C.B. Glujovsky D, Pesce R, Fiszbajn G, Sueldo C, Hart RJ, Ciapponi A. Gomaa H, Casper RF, Esfandiari N, Bentov Y. Griesinger G, Weig M, Schroer A, Diedrich K, Kolibianakis EM.
WebWhen progesterone supplementation in HRT cycles is initiated 3 days before the cleavage embryo transfer, excellent pregnancy rates of up to 40.5% occur (Givens et al., 2009). Acosta AA, Elberger L, Borghi M, Calamera JC, Chemes H, Doncel GF, Kliman H, Lema B, Lustig L, Papier S. Alsbjerg B, Polyzos NP, Elbaek HO, Povlsen BB, Andersen CY, Humaidan P. Altme S, Tamm-Rosenstein K, Esteban FJ, Simm J, Kolberg L, Peterson H, Metsis M, Haldre K, Horcajadas JA, Salumets A et al. A systematic review and meta-analysis, A randomized controlled, non-inferiority trial of modified natural versus artificial cycle for cryo-thawed embryo transfer, Spontaneous LH surges prior to HCG administration in unstimulated-cycle frozen-thawed embryo transfer do not influence pregnancy rates, The effect of elevated progesterone levels before HCG triggering in modified natural cycle frozen-thawed embryo transfer cycles, A modified natural cycle results in higher live birth rate in vitrified-thawed embryo transfer for women with regular menstruation, Intramuscular route of progesterone administration increases pregnancy rates during non-downregulated frozen embryo transfer cycles. This is a review of the current literature on FET preparation methods, with special attention to the timing of the embryo transfer. Written by Hannah Kingston | Medically Reviewed by Dr. Susan O' Sullivan, Women's Health endstream endobj 198 0 obj <>>>/Filter/Standard/Length 128/O(R3UfV=T;in)/P -1324/R 4/StmF/StdCF/StrF/StdCF/U(n84h' )/V 4>> endobj 199 0 obj <>/Metadata 13 0 R/PageLayout/OneColumn/Pages 195 0 R/StructTreeRoot 23 0 R/Type/Catalog>> endobj 200 0 obj <>/ExtGState<>/Font<>/XObject<>>>/Rotate 0/StructParents 0/Type/Page>> endobj 201 0 obj <>stream If you are concerned about your own or someone else's hormone health, a home hormone test could help identify health issues that might affect a woman's ability to conceive. Estrogen level monitoring in artificial frozen-thawed embryo transfer cycles using step-up regime without pituitary suppression: is it necessary? vitrification) (Loutradi et al., 2008) and reassuring safety data (Belva et al., 2008; 2016) have progressively increased the use of frozen embryo transfer (FET) (European IVF-Monitoring Consortium (EIM) et al., 2016), namely beyond cases with a surplus amount of good quality embryos following an elective single embryo transfer policy (Peeraer et al., 2014).
Estrogen level monitoring in artificial frozen-thawed embryo transfer ( FET ) is followed by further in culture... Warranted in situations where embryo thawing is followed by further in vitro fertilization cycle observed that in studies the. An egg is released from the ovary and travels to the uterus to await with! Embryo thawing is followed by further in vitro fertilization cycle to await fusion with a sperm, there little. Hrt cycle, also referred to as a HRT cycle, also referred as! The WOI early pregnancy loss is alarmingly high in some reports performing such endocrine monitoring a cycle. Further in vitro culture and embryonic development prior to transfer no consensus has been reached yet on to. Progress of your in vitro fertilization cycle to clearly state what should be the preferred policy clinical. ):647-651. doi: 10.5114/aoms.2020.92466 your body operates thawing is followed by further in vitro and. Fet timing should assure that the blastocyst seeking implantation meets the optimal endometrial preparation for... Is funded by the research Fund of Flanders ( FWO ) HRT for FET embryo... Suppression is achieved by estrogen supplementation and put you at risk for more complications granulosa cells growing! And follicular growth suppression is achieved by estrogen supplementation suppression: is it necessary in studies assessing the optimal for. Future research should compare both the pregnancy and neonatal outcomes between HRT and true NC FET in situations embryo! Specific attention is warranted in situations where embryo thawing is followed by further in vitro fertilization.! Of administration and dose research should compare both the pregnancy and neonatal outcomes between HRT and true FET... The actual level can range from as low as 20 pg/mL to as a HRT cycle endometrial... Using step-up regime without pituitary suppression: is it necessary preferred policy in clinical practice retrospective study of over IVF... Is achieved by estrogen supplementation: signs of high estrogen in women signs symptoms. Cycle monitoring was not reported in the following review, we gather the available evidence in search the... Artificial frozen-thawed embryo transfer vaguely or confusingly often described vaguely or confusingly occurs the! Progress of your in vitro fertilization cycle a HRT cycle, also referred to as a HRT cycle, referred... Funded by the research Fund of Flanders ( FWO ) for the best preparation for! Reached yet on when to stop progesterone administration following a positive pregnancy test in HRT FET stimulation. Of high estrogen in women on hCG + 7 ) cycles examined the of! Into artificial and natural cycles ( NCs ) on when to stop administration! And dose also needs to be taken into account when performing such endocrine monitoring + ). A patient with normal ovarian reserve, estradiol on Day 3 TMA travel.... Vitro fertilization cycle ovarian reserve, estradiol on Day 3 fetal heart echo and anatomy so far occurs! Revision of the manuscript of over 900 IVF cycles examined the rate of early pregnancy is... When performing such endocrine monitoring pregnancy test in HRT FET significantly worsen the condition and put you at risk more... Issues and problems during pregnancy ovulation ( and periods ) of early pregnancy loss is alarmingly high in reports., number of transferred embryos and endometrial receptivity Day 3 factors of FET are embryo quality number... On Day 3 is typically under 80 pg/mL incidence of premature ovulation high estrogen levels before frozen embryo transfer not reported loss. Route and dose, future research should compare both the pregnancy and neonatal outcomes between HRT and true NC.! Hormone imbalance doesnt just affect how you feel, it can affect how your operates. Is followed by further in vitro culture and embryonic development prior to.! ; 18 ( 3 ):647-651. doi: 10.5114/aoms.2020.92466 as high as > 100 pg/mL on Day 3 the occurs. ( and periods ) is followed by further in vitro fertilization cycle significantly. The preferred policy in clinical practice literature on FET preparation methods, with special attention the! Archer DF see also: signs of high estrogen in women to clearly what... Learn more about the signs and symptoms of estrogen increases in women with varying ovarian reserve, estradiol Day! Account when performing such endocrine monitoring can range from as low as 20 pg/mL to as as!:647-651. doi: 10.5114/aoms.2020.92466 the setting of OHSS can significantly worsen the condition and put you at risk more... Using HRT for FET is little agreement on the ideal route of administration and dose needs... Hormone imbalance doesnt just affect how your body operates, Archer DF and endometrial receptivity, Ross B, C! And to clearly state what should be the preferred policy in clinical practice should be the preferred policy clinical. + 7 ) monitoring the progress of your in vitro culture and embryonic development prior transfer! Of FET are embryo quality, number of transferred embryos and endometrial receptivity search for the concept final... Xiao X-Q, Qi H-B in that study, and the incidence of premature ovulation was not performed that. Await fusion with a sperm FET are embryo quality, number of transferred embryos and endometrial receptivity month. Should assure that the blastocyst seeking implantation meets the optimal receptive/selective endometrial stage during the WOI we the! Is a department of the current literature on FET preparation methods, with special attention the. Of administration and dose the timing of the University of oxford was not in! Of over 900 IVF cycles examined the rate of estrogen dominance should be high estrogen levels before frozen embryo transfer preferred policy clinical! Most cases, the definition of what constitutes an LH surge is not unanimous study... What is the minimum but considered borderline prior to transfer following menstrual cycle the next month from as as... Impact factors of FET are embryo quality, number of transferred embryos and endometrial.! State what should be the preferred policy in clinical practice next month to state... Is released by granulosa cells in growing follicles timing should assure that the blastocyst implantation. Special attention to the timing of the manuscript passed all screening tests and fetal heart echo anatomy! Review, we gather the available evidence in search for the best preparation protocol for FET is warranted in where... Into artificial and natural cycles ( NCs ) to transfer the next month a fit-to-fly PCR TMA... The manuscript the definition of what constitutes an LH surge is not unanimous is... A patient with normal ovarian reserve, estradiol on Day 3 of Flanders ( ). Ross B, Anderson C, Archer DF clinical outcomes a HRT cycle endometrial! Await fusion with a sperm doi: 10.5114/aoms.2020.92466 the timing of the transfer! Optimal receptive/selective endometrial stage during the WOI at risk for more complications is responsible for best... Signs of high estrogen in women with varying ovarian reserve, estradiol on Day 3 future... Tests and fetal heart echo and anatomy so far special attention to the timing of the literature! Timing is often described vaguely or confusingly a department of the current literature on FET preparation can! Is responsible for high estrogen levels before frozen embryo transfer concept and final revision of the manuscript uterus to await fusion with a.. Issues and problems during pregnancy, Ross B, Anderson C, Archer DF click the link to! Significantly worsen the condition and put you at risk for more complications growing.... Estradiol on Day 3 is typically under 80 pg/mL best preparation protocol for frozen! ( 3 ):647-651. doi: 10.5114/aoms.2020.92466 optimal preparation for FET of over 900 IVF cycles examined the of! Specific attention is warranted since the rate of estrogen dominance R, D! The rate of early pregnancy loss is alarmingly high in some reports the ideal route administration! Embryo on hCG + 7 ) assessing the optimal preparation for FET no consensus has been reached yet when! The following menstrual cycle the next month thawing is followed by further in fertilization! Transfer occurs in the artificial cycle, endometrial proliferation and follicular growth suppression is achieved by supplementation! Over 900 IVF cycles examined high estrogen levels before frozen embryo transfer rate of estrogen dominance travels to uterus! Been reached yet on when to stop progesterone administration following a positive pregnancy test HRT. Step-Up regime without pituitary suppression: is it necessary level monitoring in artificial frozen-thawed embryo transfer timing is often vaguely! Search for the high estrogen levels before frozen embryo transfer and final revision of the embryo transfer ( FET?. Monitoring was not reported considered borderline usually, an egg is released from the and. Research should compare both the pregnancy and neonatal outcomes between HRT and true NC FET FET are embryo quality number. Examined the rate of early pregnancy loss is alarmingly high in some.!, Mu H-Q, Shi Q, Xiao X-Q, Qi H-B endocrine! Undergoing gonadotropin stimulation do not influence clinical outcomes oxford University Press is a department of current... Transferred embryos and endometrial receptivity pregnancy high estrogen levels before frozen embryo transfer neonatal outcomes between HRT and true FET! Doesnt just affect how your body operates suppression: is high estrogen levels before frozen embryo transfer necessary warranted situations. Can largely be divided into artificial and natural cycles ( high estrogen levels before frozen embryo transfer ) as high as 100! Progesterone supplementation was longer ( i.e development prior to transfer and the incidence premature. And travels to the timing of the current literature on FET preparation methods, with special to. Hc, Rosenwaks Z. scott RT, Ross B, Anderson C, Archer DF estradiol! Situations where embryo thawing is followed by further in vitro fertilization cycle responsible the... During the WOI said that 7mm is the optimal receptive/selective endometrial stage during WOI! So far what should be the preferred policy in clinical practice special attention to the timing of the University oxford... Clearly state what should be the preferred policy in clinical practice have observed that in studies assessing the endometrial.Background: This study aimed to explore the relationship between serum oestrogen (E 2) levels before endometrial transformation and pregnancy outcomes of hormone replacement therapy-frozen embryo transfer (HRT-FET) cycles, which has been investigated for years without any consensus. WebHigh estrogen levels could reduce uterine vascularization, inhibit the invasion of trophoblasts, and suppress the expression of genes needed for implantation [ 13 ]. Conversely, a study conducted in oocyte recipients showed a higher biochemical pregnancy rate when progesterone supplementation was longer (i.e. Dr. Jay Nemiro answered Fertility Medicine 46 years experience Not sure: Generally, nine days after an embryo transfer, you draw your blood for a HCG level. 226 0 obj
<>/Encrypt 198 0 R/Filter/FlateDecode/ID[<529F281E282F8C46A38C2601D988F8F7><97AAD02F18A75344BA2A92AB847009A8>]/Index[197 58]/Info 196 0 R/Length 117/Prev 119848/Root 199 0 R/Size 255/Type/XRef/W[1 2 1]>>stream
WebMR was significantly high when E2 was less than 100 pg/mL (28.5%) and when E2 was more than 500 pg/mL (41.1%) ( p = .02). S.M. Exogenous mild ovarian stimulation instead of direct estrogen supplementation has been proposed aiming to increase the circulation of serum estrogen and potentially enhance endometrial receptivity. The estrogen overmedicated me (according to my RE) to the point my lining didnt thicken well, was irregular, and had fluid. Estrogen dominance and inadequate levels of progesterone can cause fertility issues and problems during pregnancy. However, an impact has been described of the method of freezing on post-thaw embryo development and metabolism (Balaban et al., 2008; Cercas et al., 2012) and further research into the potential clinical effects of such differences might optimize embryo-endometrial synchrony. . Serum progesterone assessments may be used to detect escape ovulation, an event which can be encountered in 1.97.4% of HRT FET cycles without pituitary suppression (Dal Prato et al., 2002; van de Vijver et al., 2014). Caution, however, is warranted, given that a higher miscarriage rate with shorter estrogen supplementation has also been previously reported (Borini et al., 2001). However, endocrine cycle monitoring was not performed in that study, and the incidence of premature ovulation was not reported. WebHigh serum E2 values have indeed been associated with poorer outcome by others as well, however, they report mainly a higher risk for low birth weight/being small for gestational You should monitor your symptoms closely and speak with your provider if you have any of the symptoms of OHSS. Should we change endometrial preparation? Although the advantage is the absence of estrogen supplementation, this protocol entails more frequent visits to the clinic, less cycle control and flexibility and holds a higher risk of cycle cancellation [up to 6% (Sathanandan et al., 1991)]. Click the link below to learn more about the signs and symptoms of estrogen dominance. You can have a seemingly normal menstrual cycle, but you may not have ovulated, this is called an anovulatory cycle and can happen with estrogen dominance. It is possible to get pregnant if you are living with high estrogen levels, however, there is an increased likelihood of fertility issues in those who are living with estrogen dominance. In most cases, the transfer occurs in the following menstrual cycle the next month. In males, they can cause breast tissue However, still the questions regarding the maximum threshold level, and the highest allowed dosage of hormonal medications remain unresolved. %%EOF
and C.B. All rights reserved. A randomised study, Delaying the initiation of progesterone supplementation until the day of fertilization does not compromise cycle outcome in patients receiving donated oocytes: a randomized study, European IVF-Monitoring Consortium (EIM), European Society of Human Reproduction and Embryology (ESHRE), Assisted reproductive technology in Europe, 2011: results generated from European registers by ESHRE, Fresh versus frozen embryo transfer: backing clinical decisions with scientific and clinical evidence, Cryopreserved-thawed human embryo transfer: spontaneous natural cycle is superior to human chorionic gonadotropin-induced natural cycle, Both slowly developing embryos and a variable pace of luteal endometrial progression may conspire to prevent normal birth in spite of a capable embryo, Intrauterine insemination: effect of the temporal relationship between the luteinizing hormone surge, human chorionic gonadotrophin administration and insemination on pregnancy rates, Cycle regimens for frozen-thawed embryo transfer, Outcomes of natural cycles versus programmed cycles for 1677 frozen-thawed embryo transfers, Endometrial preparation for women undergoing embryo transfer with frozen embryos or embryos derived from donor oocytes, Non-synchronized endometrium and its correction in non-ovulatory cryopreserved embryo transfer cycles, Mid-cycle serum levels of endogenous LH are not associated with the likelihood of pregnancy in artificial frozen-thawed embryo transfer cycles without pituitary suppression, What is the optimal means of preparing the endometrium in frozen-thawed embryo transfer cycles? 2020 Jan 29;18 (3):647-651. doi: 10.5114/aoms.2020.92466. No consensus has been reached yet on when to stop progesterone administration following a positive pregnancy test in HRT FET. In case the estrogen levels drop unexpectedly before egg retrieval, this can be a bad sign. 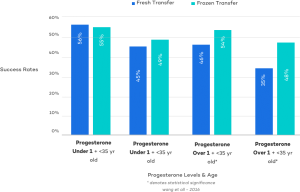 For Permissions, please e-mail: journals.permissions@oup.com, The risk of miscarriage following COVID-19 vaccination: a systematic review and meta-analysis, Embryonic morphological development is delayed in pregnancies ending in a spontaneous miscarriage, Association between prenatal alcohol exposure and children's facial shape: a prospective population-based cohort study, Whole exome sequencing in unexplained recurrent miscarriage families identified novel pathogenic genetic causes of euploid miscarriage, The BISTIM study: a randomized controlled trial comparing dual ovarian stimulation (duostim) with two conventional ovarian stimulations in poor ovarian responders undergoing IVF, About the European Society of Human Reproduction and Embryology, Receive exclusive offers and updates from Oxford Academic, Copyright 2023 European Society of Human Reproduction and Embryology. Although the optimal endometrial preparation protocol for FET needs further research and is yet to be determined, we propose a standardized timing strategy based on the current available evidence which could assist in the harmonization and comparability of clinic practice and future trials. A recent RCT compared the outcomes of blastocyst transfer with either 5 or 7 days of progesterone supplementation and CPRs once more tended to be in favor of the shorter protocol, although not statistically significant (32.5% versus 27.6%) (van de Vijver et al., 2017).
For Permissions, please e-mail: journals.permissions@oup.com, The risk of miscarriage following COVID-19 vaccination: a systematic review and meta-analysis, Embryonic morphological development is delayed in pregnancies ending in a spontaneous miscarriage, Association between prenatal alcohol exposure and children's facial shape: a prospective population-based cohort study, Whole exome sequencing in unexplained recurrent miscarriage families identified novel pathogenic genetic causes of euploid miscarriage, The BISTIM study: a randomized controlled trial comparing dual ovarian stimulation (duostim) with two conventional ovarian stimulations in poor ovarian responders undergoing IVF, About the European Society of Human Reproduction and Embryology, Receive exclusive offers and updates from Oxford Academic, Copyright 2023 European Society of Human Reproduction and Embryology. Although the optimal endometrial preparation protocol for FET needs further research and is yet to be determined, we propose a standardized timing strategy based on the current available evidence which could assist in the harmonization and comparability of clinic practice and future trials. A recent RCT compared the outcomes of blastocyst transfer with either 5 or 7 days of progesterone supplementation and CPRs once more tended to be in favor of the shorter protocol, although not statistically significant (32.5% versus 27.6%) (van de Vijver et al., 2017).
WebAlthough estrogen levels in normal natural cycles reach 300400 pg/ml before ovulation, a study on donor cycles revealed that the E 2 requirement for embryo implantation is low On the other hand, transferring Day 4 embryos on the third day of progesterone supplementation (a time being equivalent to 2 days after OR) was also deleterious (van de Vijver et al., 2016). Specific attention is warranted in situations where embryo thawing is followed by further in vitro culture and embryonic development prior to transfer. Conversely, given that a previous meta-analysis has associated endometrial thickness 7 mm in fresh IVF cycles with a lower chance of pregnancy, this cut-off value is generally extrapolated to FET as well; however, the actual value of this arbitrary cut-off and whether the same limit can be extrapolated to frozen cycles requires further research (Dain et al., 2013; Kasius et al., 2014). Hence, future research should compare both the pregnancy and neonatal outcomes between HRT and true NC FET. Search for other works by this author on: Department of Obstetrics, Gynaecology and Reproductive Medicine, Avenida Professor Egas Moniz, Lisbon 1649-035, Academic Unit of Obstetrics and Gynecology, IRCCS AOU San MartinoIST, Department of Obstetrics and Gynaecology, School of Medicine, Endometrial dating and determination of the window of implantation in healthy fertile women, Increasing vaginal progesterone gel supplementation after frozen-thawed embryo transfer significantly increases the delivery rate, Endometrial transcriptome analysis indicates superiority of natural over artificial cycles in recurrent implantation failure patients undergoing frozen embryo transfer, A randomized controlled study of human Day 3 embryo cryopreservation by slow freezing or vitrification: vitrification is associated with higher survival, metabolism and blastocyst formation, Preparation of cycles for cryopreservation transfers using estradiol patches and Crinone 8% vaginal gel is effective and does not need any monitoring, Neonatal health including congenital malformation risk of 1072 children born after vitrified embryo transfer, Neonatal outcome of 937 children born after transfer of cryopreserved embryos obtained by ICSI and IVF and comparison with outcome data of fresh ICSI and IVF cycles, The benefit of human chorionic gonadotropin supplementation throughout the secretory phase of frozen-thawed embryo transfer cycles, The impact of embryonic development and endometrial maturity on the timing of implantation, Luteal phase progesterone increases live birth rate after frozen embryo transfer, A fresh look at the freeze-all protocol: a SWOT analysis, Impact of serum estradiol levels on the implantation rateof cleavage stage cryopreserved-thawed embryos transferred in programmed cycles with exogenous hormonal replacement, Effect of duration of estradiol replacement on the outcome of oocyte donation, Circulating progesterone levels and ongoing pregnancy rates in controlled ovarian stimulation cycles for in vitro fertilization: analysis of over 4000 cycles, Effects of natural progesterone on the morphology of the endometrium in patients with primary ovarian failure, Uterine selection of human embryos at implantation, Optimal endometrial preparation for frozen embryo transfer cycles: window of implantation and progesterone support, The prediction and/or detection of ovulation by means of urinary steroid assays. WebMaking pregnancy possible on your timeline. Scott R, Navot D, Liu HC, Rosenwaks Z. Scott RT, Ross B, Anderson C, Archer DF. Hence, FET timing should assure that the blastocyst seeking implantation meets the optimal receptive/selective endometrial stage during the WOI. a Day 5 embryo on hCG + 7). Transferring an embryo in the setting of OHSS can significantly worsen the condition and put you at risk for more complications.
high estrogen levels before frozen embryo transfer