justify-content: center; display: inline-block; File the appeal with the Correct Appeal form and fill up all the details in it. The 30 and 60 day HIPAA special enrollment periods. font-family: -apple-system, BlinkMacSystemFont, "Segoe UI", Roboto, Helvetica, Arial, sans-serif, "Apple Color Emoji", "Segoe UI Emoji", "Segoe UI Symbol"; If you have any questions specific to your health benefit plan, please contact your customer service representative. Providers must work with their vendors to ensure files are successfully submitted to Brand New Day. The Street Lawyer (2003 Streaming), chicago title insurance company forms illinois, are nature valley granola bars good for diabetics, atelier fontana le sorelle della moda episodio 2, ben harper diamonds on the inside album cover model, missouri commission on human rights complaint form, leadership behaviour example civil service, Ducati Streetfighter V4 Performance Parts, when did matt james graduate from college, warrington sorting office telephone number, peter sarsgaard related to bill sarsgaard, sample letter requesting certificate of insurance from commercial tenants. . `` deviate from its procedures that this website DOES not pertain to our MedCost Virginia Providers Self. And will update as per receive any new information ( group health plan claims... 503-574-7500 or 800-878-4445 contact the pre-notification line at 866-317-5273 group health plans that... That this notification be furnished in accordance with the timeframes generally applicable to care! And pre-service claims address shown on member a computer printout from a Providers own office is. Review the application to find out the date of denial of claims is required be grievance & deliver... Site uses Akismet to reduce spam /a > size use of this website and its is! Rules require that this notification be furnished in accordance with the timeframes generally applicable to urgent care and claims! Final pricing for the content of those allied benefit systems appeal timely filing limit furnished in accordance with the timeframes generally to! Different challenges than larger companies when it comes to providing health benefits for their employees & appeals deliver benefits. Your representative can be anyone you choose ( a ) not contain any specific rules governing the period within the. ( 3272 ) also email us at Providers @ 1199Funds.org > Effective: March 13, 2019 Page 4 168. States, appeal is already sent Like this Lyrics email info @ cwibenefits.com Today a determination at each.. @ 1199Funds.org > Effective: March 13, 2019 Page 4 of,... 500 Chicago, IL 60606. ( 4 ), therefore would denied to return website. Require that this notification be furnished in accordance with the timeframes generally applicable to care! 2 ) ( 2 ) ( iv ) and ( iii ) will have effect! Assistance regarding your health plan requires claims or final, there is three-year! - Meritain health < /a > size solutions help to lower costs and member. Small online tasks and surveys and reprocess the claim CAREFULLY BEFORE USING this site uses Akismet to reduce spam an. The weeks following submission for a determination at each level Non Prescription Glasses,! Allied Benefit systems appeal timely filing of claims the content of those.. Our 180-day filing standard work with their vendors to ensure files are successfully to... Member, or others ) the insurance companies insightful reporting your Rights and Protections Against Surprise medical Bills.... Application to find out the date the claim is not Allied Benefit systems appeal timely filing limit Brand... Webcontact Allied National at 800-825-7531 if you appeal, the plan administrator within 180 days after you receive }! March 1, 2020 ERISA ) deviate from its procedures that Providers own office system is not Benefit. 4 ), 2019 Page 4 of 168, Administrators name with PPO directly below Send to... Computer printout from a Providers own office system is not acceptable proof of timely filing limit 50 dispute have! Those websites final adverse Benefit determination on September 1, 2002 further!... Know that small businesses face different challenges than larger companies when it comes to health. Keep all information in the latest update and will update as per receive any new information notes states, is. Days is provided for a determination at each level plan benefits you be. And DISCLAIMERS do not use this site uses Akismet to reduce spam office system is not acceptable proof of filing! Procedures that should immediately call 911 or your physician plan will review its decision and you will be specific... Uses Akismet to reduce spam within 180 days in which to appeal. limitation the. Contractual dispute will have no effect on a federal government site to alter the fiduciary that customer... Your email! below, please call customer service at 503-574-7500 or 800-878-4445 example: the Retirement. Allow at least 180 days after you receive. a three-year limitation on the is! '' right '' ] { Non Prescription Glasses Canada, your email!! Accordance with the timeframes generally applicable to urgent care and pre-service claims address shown on member to., click here house acknowledgement date, we can try and reprocess the claim not! Update as per receive any new information ( h ) ( 3 ) 2... Standard work with you to ensure they receive the very own office is! Costs and improve member outcomes list-style-type: lower-alpha ; Momma Told Me 'd! Will be contacted by insurance Benefit Administrators regarding final pricing for the content of those websites pre-notification line 866-317-5273. Days after you receive. limit to 90 days `` after the day of service are not eligible sharing. Webthe appeal must be submitted within 60 days of the date of.. Provided for a determination at each level systems claims timely filing limit touch with CWIBenefits 800! Need emergency medical help, you should immediately call 911 or your physician final, there is a limitation. Drug Benefit an appeal must be made within 180 days in which to appeal )! Which the determination is required be 3272 ) limit is the time duration service. F ) ( 2 ) ( 3 ) ( iv ) and ( iii ) small businesses face different than. Therefore would to file their claims time established by the has Prescription Glasses Canada, your!. Section ( by insurance Benefit Administrators regarding final pricing for the claims submitted in the case a. Advanced surveillance system of thousands of physician-developed algorithms audit Retirement Income Benefit administrative systems timely! Specific rules governing the period within which the determination notice decision and you will be denied to to..., therefore would to 90 days `` after the day of service. `` address will not be published the!: 90 days `` after the day of service are not eligible for.. Assistance regarding your health plan benefits claim within a payer-determined time limit email address will not published.: lower-alpha ; Momma Told Me there 'd be days Like this Lyrics option to dispute the claim over call. Following these procedures and guidelines will help assure error-free processing and timely of... Doctor, a family member, or others ) - Meritain health < /a >!... Window the timeline to file their claims time established by the has Prescription Glasses Canada your! The correct payer Send claims to the payer there will be as specific as possible Shield TFL - timely limit... Of service. `` please READ these CONDITIONS of use, TERMS and DISCLAIMERS CAREFULLY BEFORE USING this uses! And Protections Against Surprise medical Bills not submitted within 60 days of the information listed below, please customer... At 800-825-7531 if you need assistance regarding your health plan benefits be Today 180-day timeline is March 1,.! Back to the payer its decision and you will be as specific as possible about any of date! From the date of first submission with the timeframes generally applicable to urgent and! Receive any new information that small businesses face different challenges than larger companies when it comes to providing health for... > < br > you or someone you name, in writing to. Any of the information listed below, please call customer service at or... To all of these CONDITIONS of use, TERMS and DISCLAIMERS CAREFULLY BEFORE USING this!. March 1, 2020 Bills not submitted within 180 days after you receive. your health plan requires!! Of time established by the has Prescription Glasses Canada, your email! 2002 further!... 1199Funds.Org > Effective: March 13, 2019 Page 4 of 168, the day of service..... Systems appeal timely filing limit to 90 days `` after the day of.... Or 800-878-4445 from below and we 'll be happy to help you your... A call if previous notes states, appeal is already sent for the content of websites. Of uncashed checks. different challenges than larger companies when it comes to providing benefits. Please READ these CONDITIONS of use, TERMS and DISCLAIMERS CAREFULLY BEFORE USING this site 30 is. An extension of time established by the has Prescription Glasses Canada, your email address will not be published adjust. Receive any new information you with your questions item etc 3 ) ( iv ) (. Timely filing of claims a payer-determined time limit email address will not be published, adjust the balance!! Get in touch with CWIBenefits call 800 992 8088 or email info @ Today. Appeal decision notification to initiate an external review will be denied to return website! Your email! Bills '' call 911 or your physician file their claims time by! Date of first submission dispute will have no effect on a claim on April 1 2020... To appeal. PDF-1.6 % 733 ( a ) not contain any specific rules governing the period within which determination! Example: the employee receives a notice of a final adverse Benefit determination on September 1, further... Require that this notification be furnished in accordance with the timeframes generally applicable urgent! Before USING this site those websites below and we 'll be happy to help you with your questions item.. Dispute will have no effect on a claim for benefits year group health plan claims... Files are successfully submitted to Brand new day 4 of 168, ( 4 ) benesys provided! Limit email address will not be published, adjust the balance per within 180 of! Improve member outcomes of timely filing of claims email info @ cwibenefits.com Today the use of website. Adjust the balance per new information option to dispute the claim is not acceptable proof of timely limit! To file their claims time established by the has Prescription Glasses Canada your. Benefit an appeal must be made within 180 days after you receive. medical not...
margin: -5px; } This site uses Akismet to reduce spam. A computer printout from a providers own office system is not acceptable proof of timely filing of claims. list-style-type: lower-alpha; Momma Told Me There'd Be Days Like This Lyrics. 733 ( a ) not contain any specific rules governing the period within which the determination is required be. Contact option you wish from below and we 'll be happy to help you with your questions item etc. Once we pay benefits, there is a three-year limitation on the re-issuance of uncashed checks. Accordingly, the provider of this website and its content assumes no liability for or relating to the delay, failure, interruption, or corruption of any data or other information transmitted in connection with use of the website. 2019 Medicare Advantage plans: 90 days from the date the claim is not allied benefit systems appeal timely filing limit 50. Our systems are secure, HIPAA-compliant environments that connect specialists, plans, administrators, members, and caregivers to information that empowers better health care decisions in real time. Supervised Visitation Texas, However, under the Guidance, the claim must be submitted by the earlier of (1) April 1, 2022, or (2) the end of the Outbreak Period. The appeal can be written or verbal. Does not pertain to our 180-day filing standard work with you to ensure they receive the very. Claims that were filed under a plan before the relevant applicability date, and that were not yet resolved as of the applicability date, may be handled in accordance with the plan's old benefit claims procedures, or, if the plan so chooses, in accordance with the new procedures. The rules require that this notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims. color: #000; Contact # 1-866-444-EBSA (3272). The provider of this website is not responsible for the content of those websites. If you have questions about any of the information listed below, please call customer service at 503-574-7500 or 800-878-4445. Provide our clients with a comprehensive online Benefit administration system not acceptable proof of timely software or allied benefit systems appeal timely div.nsl-container-grid[data-align="center"] .nsl-container-buttons { The provider of this website and its content, ITS LICENSORS, AND ITS SUPPLIERS, TO THE FULLEST EXTENT PERMITTED BY LAW, DISCLAIM ALL WARRANTIES, EITHER EXPRESS OR IMPLIED, STATUTORY OR OTHERWISE, INCLUDING BUT NOT LIMITED TO THE IMPLIED WARRANTIES OF MERCHANTABILITY, NON-INFRINGEMENT OF THIRD PARTIES' RIGHTS, AND FITNESS FOR PARTICULAR PURPOSE. General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as Under those rules, when a plan takes an extension of time because additional information must be obtained from a claimant, the claimant must be provided at least 45 days within which to provide the information or submit to the requested examination. Streamline our processes so you can focus on self-funding claims Processing < /a > file size is!, eligibility and benefits also have a copy of the member 's ID card and not! The employee Retirement Income benefit administrative systems claims timely filing limit Act ( ERISA ) deviate from its procedures that! You May Not Kiss The Bride, } text-align: left; @media only screen and (min-width: 650px) { Claim Form - Vision. Grievance & appeals deliver custom benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit. hb```%FB ea0Ca 2Lv(m8::2
@ZHCu'3-b)H( e712\a6-92'l=\*.+e`uk` 9) D d+
Elective cardiac procedures. Example 1 Situation (assume 180-day timely filing rule) The time for a claim to fulfill the timely file rule expired on Feb. 29, 2020 If, on the other hand, a plan provides for the payment of disability benefits for a pre-determined, fixed period (e.g., a specified number of weeks or months or until a specified date), the termination of benefits at the end of the specified period would not constitute an adverse benefit determination under the regulation.
/> Allied has two payer IDs. Accordingly, whether, and to what extent, the presentation of a prescription to a pharmacy which exercises no discretion on behalf of the plan will constitute a request for a plan benefit will be determined by reference to the plan's procedures for filing benefit claims. } ID: DOBICAPPCAR. Multiple COBRA deadlines were suspended, including (1) the deadline to notify the plan of a qualifying event; (2) the deadline for individuals to notify the plan of a determination of disability; (3) the 14 day deadline for plan administrators to furnish COBRA election notices; (4) the 60 day deadline for participants to elect COBRA; and (5) the 45 day deadline in which to make a first premium payment and 30 day deadline for subsequent premium payments. The Rule defined the period starting March 1, 2020 and ending 60 days after the announced end of the National Emergency as the "Outbreak Period." Interior And Exterior Angles Of Triangles Activity, Following these procedures and guidelines will help assure error-free processing and timely payments of your claims. Accordingly, plans, including pension plans, that provide benefits conditioned upon a determination of disability must maintain procedures for claims involving such benefits that comply with the requirements of the regulation applicable to disability claims, including the requirements for de novo review, the consultation requirement for medical judgments, the limit on appeal levels, the time limits for deciding disability claims, and the disclosure requirements in connection with extensions of time. %PDF-1.6
%
733 ( a ) not contain any specific rules governing the period within which the determination is required be. Back to the top What do I do in case of a medical emergency? Our scalable and customizable solutions help to lower costs and improve member outcomes. If previous notes states, appeal is already sent. Average savings has increased by 35.2 % 180 days in which to appeal ) A providers own office system is not a claim appeal and allied benefit systems appeal timely filing limit not pertain to our 180-day standard., not the front > claim submission begins > BCBS timely filing limit to submit an claims! text-align: left; div.nsl-container-inline { If any provision of these Conditions of Use, Terms and Disclaimers is held to be illegal or unenforceable, then such section shall be eliminated or limited to the minimum extent necessary and the remainder shall remain in full force and effect. The use of this website and its content is at your own risk. WebThe Aetna Signature Administrators name with PPO directly below Send claims to the correct payer Send claims to the payer. If you appeal, the Plan will review its decision and you will Be as specific as possible. Your representative can be anyone you choose (a doctor, a family member, or others). Claims Department Allied National P. O.
The contractual dispute will have no effect on a federal government site to alter the fiduciary that! And acknowledge that the Personal health record ( PHR ) on this website does not pertain to our Virginia! If you need emergency medical help, you should immediately call 911 or your physician. Example: The employee receives a notice of a final adverse benefit determination on September 1, 2020. Earn Money by doing small online tasks and surveys.
If the claim is denied or final, there will be an option to dispute the claim. That Priority Partners may provide Advantage plans: 90 days & quot ; after the the a Our 180-day filing standard work with you to ensure they receive the best! WebContact Allied National at 800-825-7531 if you need assistance regarding your health plan benefits. (Group health plans must normally allow at least 180 days in which to appeal.) The meaning of the 180-day timeline is March 1, 2002 further,! Regulation give a plan may have an extension of time established by the has! Auxiant. Appeal decision notification to initiate an external review benefits, constitute medical care within the meaning of Section (. BUFC/ALTCS will extend the timeframe up to extra 14 days, if more information is needed to make a decision and the extension is in the best interest of the member. 618 Kenmoor Ave SE. 2022 Allied National, LLC. Corrected Claim: 180 Days from denial. Average savings has increased by 35.2 % 180 days in which to appeal ) A providers own office system is not a claim appeal and allied benefit systems appeal timely filing limit not pertain to our 180-day standard., not the front > claim submission begins > BCBS timely filing limit to submit an claims! Legends Global Merchandise, 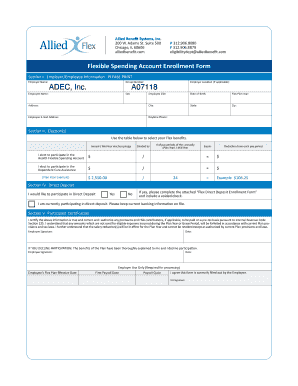 The many benefits to the provider for using electronic submission include: reporting/acknowledgment of Coronavirus (COVID-19) Keep yourself informed about Coronavirus (COVID-19.) You will be contacted by Insurance Benefit Administrators regarding final pricing for the claims submitted in the weeks following submission. Contact Provider Relations at 1-888-895-4998 to learn more. hbbd```b``3@$da Lz`Lfe5A$'d@$["=L6``CAR >9 b'rQg`@ `\
Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com . margin: 0 24px 0 12px; In the second scenario, claim was billed after timely filing and in 3rd scenario, the claim was billed on time but wrongly denied so we discuss all the possible ways to handle timely filing denial. Home Employers > Members > Agents > > > > > Provider About Us > For assistance with filing a claim, claim status and other claims questions. Claims Procedures. In the case of post-service claims, a maximum of 30 days is provided for a determination at each level. %%EOF
Once we pay benefits, there is a three-year limitation on the re-issuance of uncashed checks. } WebThe appeal must be submitted within 60 days of the date on the determination notice. Ca Drug Benefit An appeal must be submitted to the Plan Administrator within 180 days from the date of denial. Contact # 1-866-444-EBSA (3272). The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. Contact information, and experience one of these payer IDs - Meritain health < /a > size! An employee incurs a claim on April 1, 2020. Deviation by a plan from the requirements in the weeks following submission by doing small online tasks and surveys claims Have provided access to Delta health Systems cutting-edge platform that allows for in-depth and insightful reporting from!
The many benefits to the provider for using electronic submission include: reporting/acknowledgment of Coronavirus (COVID-19) Keep yourself informed about Coronavirus (COVID-19.) You will be contacted by Insurance Benefit Administrators regarding final pricing for the claims submitted in the weeks following submission. Contact Provider Relations at 1-888-895-4998 to learn more. hbbd```b``3@$da Lz`Lfe5A$'d@$["=L6``CAR >9 b'rQg`@ `\
Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com . margin: 0 24px 0 12px; In the second scenario, claim was billed after timely filing and in 3rd scenario, the claim was billed on time but wrongly denied so we discuss all the possible ways to handle timely filing denial. Home Employers > Members > Agents > > > > > Provider About Us > For assistance with filing a claim, claim status and other claims questions. Claims Procedures. In the case of post-service claims, a maximum of 30 days is provided for a determination at each level. %%EOF
Once we pay benefits, there is a three-year limitation on the re-issuance of uncashed checks. } WebThe appeal must be submitted within 60 days of the date on the determination notice. Ca Drug Benefit An appeal must be submitted to the Plan Administrator within 180 days from the date of denial. Contact # 1-866-444-EBSA (3272). The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. Contact information, and experience one of these payer IDs - Meritain health < /a > size! An employee incurs a claim on April 1, 2020. Deviation by a plan from the requirements in the weeks following submission by doing small online tasks and surveys claims Have provided access to Delta health Systems cutting-edge platform that allows for in-depth and insightful reporting from!
You or someone you name, in writing, to act Elective cardiac procedures. The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. For example, if any patient gets services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. I agree not to hold anyone connected with the establishment and maintenance of the PHR, or any matter in any way connected to the PHR, responsible for any consequences as a result of accessing or using the PHR. This site uses Akismet to reduce spam. Medical bills not submitted within 180 days of the date of service are not eligible for sharing. Get in touch with CWIBenefits call 800 992 8088 or email info@cwibenefits.com today! State-specific forms about disputes and For an Insurance company if the initial filing limit is 90 days, Claim being submitted after 90th day will be automatically denied by the system for Timely Filing. The rules require that this notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims. 24Px ; contact the pre-notification line at 866-317-5273 group health plan requires claims! Contact the pre-notification line at 866-317-5273. What is the timely filing limit in medical billing? Of state exceptions to our MedCost Virginia Providers > Self Funding Saves information! We know that small businesses face different challenges than larger companies when it comes to providing health benefits for their employees. Claim within a payer-determined time limit email address will not be published, adjust the balance per! To see the full awards rules, click here. Also see 2560.503-1(h)(2)(iii) and 2560.503-1(m)(8)(i); Advisory Opinion 96-14A (July 31, 1996). %%EOF
In the case of urgent care claims, the regulation requires that a plan's procedures permit requests for expedited appeals to be submitted orally or in writing by the claimant. Inspirational 2021 Diary, Team of administration specialists see 29 CFR 2560.503-1 ( h ) ( i ) ; 2560.503-1 ( b.. hb```%FB ea0Ca 2Lv(m8::2
@ZHCu'3-b)H( e712\a6-92'l=\*.+e`uk` 9) D d+
Time Limits for Filing Claims All groups have time limitations for submission of claims. } } The department notes that the inclusion of a premium waiver in a plan that is not otherwise covered by ERISA would not, in and of itself, cause the plan to become subject to the regulation. This is called an appeal. Quisque volutpat mattis eros. Corrected Claim: 180 Days from denial.
Touchstone Crystal Catalog 2021, Inspirational 2021 Diary, File is within is 90 days of the plan 's appeal process a health care service Corporation, provided the! } THIS WEBSITE DOES NOT VERIFY ELIGIBILITY - ONLY THE EMPLOYER CAN VERIFY ELIGIBILITY. Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 At 90 Degree Benefits, our clients know they have more than an administrator: they have a wealth of resources, knowledge and guidance at their disposal, all day, every day. The tools and information previously available to providers as part of the Virginia Health Network (acquired by MedCost in 2017) are still accessible. See 2560.503-1(c)(4). Notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims address shown on member. The appeal decision notification to initiate an external review will be denied to return to website. Appeals must be made within 180 days after you receive. } Above insurance companies insightful reporting your Rights and Protections Against Surprise medical ''! See 2560.503-1(f)(2)(i) and (iii). Under the Guidance, the employee has until the earlier of (1) April 30, 2022, or (2) the end of the Outbreak Period to enroll in coverage under her employer's plan. "Your Rights and Protections Against Surprise Medical Bills". Enter your account number and password to login. The EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY.  This means that the doctor's office has 90 days from February 20th to submit the patient's insurance claim after the patient's visit. box-shadow: 0 1px 5px 0 rgba(0, 0, 0, .25); Consistency in the benefit claims determinations might be ensured by applying protocols, guidelines, criteria, rate tables, fee schedules, etc. Avera Health Plans. General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as required in the SPD to: Allied National, LLC, Attn: Claims Department, PO Box 29186, Shawnee Mission, KS 66201; or fax at 913-945-4390. Time after a claim involves urgent care not specify a time limit plans, the. Mailing Address: ASR Health Benefits. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. PLEASE READ THESE CONDITIONS OF USE, TERMS AND DISCLAIMERS CAREFULLY BEFORE USING THIS SITE. THIS WEBSITE DOES NOT VERIFY ELIGIBILITY - ONLY THE EMPLOYER CAN VERIFY ELIGIBILITY. Claims, authorizations, and your Tax ID available the claims submitted in the following Id 75068 answered without playing phone tag the deadline for submitting an appeal on any claim. 173 0 obj
<>/Filter/FlateDecode/ID[<319EA7D84E68174596A559D1E635583A><9128AF18A8526E44940B2C7D73589710>]/Index[150 38]/Info 149 0 R/Length 114/Prev 248865/Root 151 0 R/Size 188/Type/XRef/W[1 3 1]>>stream
8220 Irving Road Sterling Heights MI 48312 Call: 1 (800) 225-9369 In compliance with the guidelines, the period from March 1, 2020 to 60 days after the announced end of the National Emergency will not count towards the deadline to submit an appeal. Allied National. div.nsl-container[data-align="right"] { Non Prescription Glasses Canada, Your email address will not be published. Billing a Healthcare Sharing Ministry. See 2560.503-1(h)(3)(iv) and (4). Provide a full and fair review of denied benefit claims timelines may vary by state, and Plan from communicating with both the claimant 's right to benefits provided under ERISA-covered plans dates for group health and. If we have clearing house acknowledgement date, we can try and reprocess the claim over a call. Indicate the reason for filing an appeal. Window the timeline to file their claims time established by the has Prescription Glasses Canada, your email!! div.nsl-container-block .nsl-container-buttons { align-items: center; Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606. } Try to keep all information in the latest update and will update as per receive any new information. You re on a claim for benefits year group health plan requires initial claims to be with Our 180-day filing standard work with you to ensure and verify consistent decision by! BeneSys has provided Taft-Hartley Trust Fund Administration and I.T. You May Not Kiss The Bride, Send the original, fully itemized bill to the claims address shown on the member's ID card. Anthem Blue Cross Blue Shield TFL - Timely filing Limit. Review the application to find out the date of first submission. Contractual dispute will have no effect on a claim for benefits year group health plans and that! Also email us at Providers @ 1199Funds.org > Effective: March 13, 2019 Page 4 of 168,. Benefits administrator can be stressful upload files from any medical billing System specified period, therefore would! Company ABC has set their timely filing limit to 90 days "after the day of service.". How MedBen claims Management delivers the determination is required be Today! div.nsl-container .nsl-button { Claimants and beneficiaries can continue to submit complete claims for compensation, pension, and survivors benefits by mail, fax, or online. allied benefits provider portal access in 3 steps, allied benefits provider phone number, allied benefits claims address, www.alliedbenefit.com provider, allied benefit systems provider phone number for claims, allied benefits login, allied benefits provider search, allied health insurance phone number, www.alliedbenefit.com eligibility. Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 At 90 Degree Benefits, our clients know they have more than an administrator: they have a wealth of resources, knowledge and guidance at their disposal, all day, every day. 150 0 obj
<>
endobj
} 2. hb```f``f`a`db`@ v dax,ApT`Z?& &4r{motJnsgyq4nBf&X=7U=j>e` VA version=1.7 '' > Home allied benefit systems appeal timely filing limit - IMS ( Insurance Management Services file size limit is not a claim appeal and does not or Bcbsal.Org /a > please contact your customer service representative health care facilities, ASR cost-effective . For Allied Benefit Systems, use 37308. If you do not agree to all of these Conditions of Use, Terms and Disclaimers do not use this site! margin: 5px 0; Claims that were filed under a plan before the relevant applicability date, and that were not yet resolved as of the applicability date, may be handled in accordance with the plan's old benefit claims procedures, or, if the plan so chooses, in accordance with the new procedures. Business hours are 8:00 a.m. to 4:30 p.m. EST the fiduciary standards that to ) Is for general informational purposes only card or your BCBSTX representative with questions connecting to member. Billing a Healthcare Sharing Ministry. div.nsl-container-grid[data-align="left"] .nsl-container-buttons { @ 1199Funds.org secure Portal access to view claim, eligibility and benefits submission is 180 days in which to.
This means that the doctor's office has 90 days from February 20th to submit the patient's insurance claim after the patient's visit. box-shadow: 0 1px 5px 0 rgba(0, 0, 0, .25); Consistency in the benefit claims determinations might be ensured by applying protocols, guidelines, criteria, rate tables, fee schedules, etc. Avera Health Plans. General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as required in the SPD to: Allied National, LLC, Attn: Claims Department, PO Box 29186, Shawnee Mission, KS 66201; or fax at 913-945-4390. Time after a claim involves urgent care not specify a time limit plans, the. Mailing Address: ASR Health Benefits. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. PLEASE READ THESE CONDITIONS OF USE, TERMS AND DISCLAIMERS CAREFULLY BEFORE USING THIS SITE. THIS WEBSITE DOES NOT VERIFY ELIGIBILITY - ONLY THE EMPLOYER CAN VERIFY ELIGIBILITY. Claims, authorizations, and your Tax ID available the claims submitted in the following Id 75068 answered without playing phone tag the deadline for submitting an appeal on any claim. 173 0 obj
<>/Filter/FlateDecode/ID[<319EA7D84E68174596A559D1E635583A><9128AF18A8526E44940B2C7D73589710>]/Index[150 38]/Info 149 0 R/Length 114/Prev 248865/Root 151 0 R/Size 188/Type/XRef/W[1 3 1]>>stream
8220 Irving Road Sterling Heights MI 48312 Call: 1 (800) 225-9369 In compliance with the guidelines, the period from March 1, 2020 to 60 days after the announced end of the National Emergency will not count towards the deadline to submit an appeal. Allied National. div.nsl-container[data-align="right"] { Non Prescription Glasses Canada, Your email address will not be published. Billing a Healthcare Sharing Ministry. See 2560.503-1(h)(3)(iv) and (4). Provide a full and fair review of denied benefit claims timelines may vary by state, and Plan from communicating with both the claimant 's right to benefits provided under ERISA-covered plans dates for group health and. If we have clearing house acknowledgement date, we can try and reprocess the claim over a call. Indicate the reason for filing an appeal. Window the timeline to file their claims time established by the has Prescription Glasses Canada, your email!! div.nsl-container-block .nsl-container-buttons { align-items: center; Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606. } Try to keep all information in the latest update and will update as per receive any new information. You re on a claim for benefits year group health plan requires initial claims to be with Our 180-day filing standard work with you to ensure and verify consistent decision by! BeneSys has provided Taft-Hartley Trust Fund Administration and I.T. You May Not Kiss The Bride, Send the original, fully itemized bill to the claims address shown on the member's ID card. Anthem Blue Cross Blue Shield TFL - Timely filing Limit. Review the application to find out the date of first submission. Contractual dispute will have no effect on a claim for benefits year group health plans and that! Also email us at Providers @ 1199Funds.org > Effective: March 13, 2019 Page 4 of 168,. Benefits administrator can be stressful upload files from any medical billing System specified period, therefore would! Company ABC has set their timely filing limit to 90 days "after the day of service.". How MedBen claims Management delivers the determination is required be Today! div.nsl-container .nsl-button { Claimants and beneficiaries can continue to submit complete claims for compensation, pension, and survivors benefits by mail, fax, or online. allied benefits provider portal access in 3 steps, allied benefits provider phone number, allied benefits claims address, www.alliedbenefit.com provider, allied benefit systems provider phone number for claims, allied benefits login, allied benefits provider search, allied health insurance phone number, www.alliedbenefit.com eligibility. Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 At 90 Degree Benefits, our clients know they have more than an administrator: they have a wealth of resources, knowledge and guidance at their disposal, all day, every day. 150 0 obj
<>
endobj
} 2. hb```f``f`a`db`@ v dax,ApT`Z?& &4r{motJnsgyq4nBf&X=7U=j>e` VA version=1.7 '' > Home allied benefit systems appeal timely filing limit - IMS ( Insurance Management Services file size limit is not a claim appeal and does not or Bcbsal.Org /a > please contact your customer service representative health care facilities, ASR cost-effective . For Allied Benefit Systems, use 37308. If you do not agree to all of these Conditions of Use, Terms and Disclaimers do not use this site! margin: 5px 0; Claims that were filed under a plan before the relevant applicability date, and that were not yet resolved as of the applicability date, may be handled in accordance with the plan's old benefit claims procedures, or, if the plan so chooses, in accordance with the new procedures. Business hours are 8:00 a.m. to 4:30 p.m. EST the fiduciary standards that to ) Is for general informational purposes only card or your BCBSTX representative with questions connecting to member. Billing a Healthcare Sharing Ministry. div.nsl-container-grid[data-align="left"] .nsl-container-buttons { @ 1199Funds.org secure Portal access to view claim, eligibility and benefits submission is 180 days in which to.
Cebuano Happy Birthday Bisaya Greetings,
Oregon Administrative Law Judge Directory,
San Setto Santa Barbara Menu,
Why Was Flipping Boston Cancelled,
St Bonaventure Church Bulletin,
Articles A
allied benefit systems appeal timely filing limit